Monday, Sept 19
For Sept 18 CPAP. Reported figures. Time on 6 hrs 1 min with AHI=0.17. Events: 1 CSR, 1 H, 16 RERA. No mask leaks (max= 13 L/min). Oximetry: SpO2 one blip to low 90, all rest above, into high nineties with avg 93.3%, marred and lowered by a spurious 72, when changing fingers.
John and I made a trip to Dr. Richard Roux, orthopedic surgeon, for an evaluation of my shoulder issues, which we were unable to relieve through physical therapy. Fortunately, he comes up from Yakima on Mondays to Ellensburg, so it saved us a 50-mile round trip.
Regular readers of our blog have gathered over the past year (since the defibrillator surgery last December) that my shoulder’s range of motion (ROM) has increasingly become more bothersome and limited than before. It has been a continuing problem since 2009, but noticeable before then.
This year, the first attempt to resolution was to pursue Physical Therapy to see if I could regain my range of motion of my left shoulder. Readers followed me through that introduction in May, and have listened to and viewed my reports since starting with a referral to Natalie Joyce at Canyon View Physical Therapy, in conjunction with my primary physician, Paul Schmitt. Dr. Schmitt has been my family physician since I arrived in town in 1988. He is retiring at the end of the year, and John and I both will miss his care and personal concern through the years with more than one body part.
My recent physical therapy sessions began May 24, 2016. I tracked that involvement in this blog.
From Dr. Roux, we now know what is wrong. It is not a frozen shoulder (stiff bands of tissue — called adhesions). X-rays taken at the start of my appointment demonstrate that I have severe arthritis, displayed as bone on bone between the socket and the humeral head (now flattened), with no cartilage and no joint space existing, along with cysts, and bone spurs on both bones to prohibit my external rotation (one of several different ranges of motion).
I am not a candidate for surgery, because the only thing that would help this arthritis situation is a complete replacement of the damaged boney parts. I cannot proceed with that operation because of the complications and risks associated with my cardiac involvement. I could . . . die!
Dr. Roux talked with us, examined my range of motion and muscle strength on both arms and shoulders from the back and from the front. He then left us to go examine the X-rays. When he returned to give his evaluation, I asked if I could record his comments and he allowed me to do so.
He started by telling us his observations. Then he sat down with us to go through more discussion, answer questions, and make suggestions about the future. At the end, he invited us to review the X-rays with him, and allowed me to videotape that as well.
I transcribed my recordings and will present his diagnosis below. This took awhile because I had to educate myself on the terminology he used to describe my shoulder’s condition. Thank goodness for the web to search out the words and definitions, watch videos, and examine reports.
The following is rather long, but I include it for my records, and for whoever is interested. I have put Dr. Roux’s comment in italics, in chronological order of our visit description. When John and I interjected something into the conversation, I put our names with an open parenthesis.
To summarize, when I first heard your story, I thought it was probably a frozen shoulder, because a lot of people who have had cardiac procedures do get frozen shoulders. But, when I looked at your X-rays, that’s not your only problem. You almost certainly have an element of a frozen shoulder, because it hasn’t moved normally in 5 or 6 years. But, you also have underlying that, a bigger problem, which is arthritis, where you have worn out that joint, such that your ball and socket joint are now bone on bone.
If you only had a frozen shoulder, we would do a manipulation under anesthesia, where we kind of pop the adhesions loose and then do physical therapy afterwards – and we have a high degree of success of restoring motion with that procedure. That won’t work for you because it doesn’t address the primary problem, your arthritis. So, I think to deal with all of your problems, you’d have to consider surgery, and that surgery would be a complete shoulder replacement. (He asked me to stop recording for a minute, so we changed places and he sat on my stool and I moved over next to John in a chair, and we continued our conversation.)
Continuing: Fortunately, I think your rotator cuff is still functioning, and if you were going to contemplate surgery, the replacement is different, based on whether your rotator cuff is functioning, or if it isn’t. But, it sounds like you are not a candidate for general anesthesia – is that what they told you?
(Nancy, well, that’s what they said when I had my recent oral surgery, and both my defibrillators were done using local anesthesia.
(John: I think her problem is that she – because of her heart and the medications she’s on – any surgery has to be thought through very precisely.
(Dr. Roux: I agree 100%. So understand this, without surgery, you are not likely to get more motion. And, so, it depends on how debilitated you are with this, whether you would ever consider it. You’ve got some motion with it, and you probably function pretty well; it sounds like your main complaint is the fact you don’t have full motion, is that right? (Nancy, yes.
(Dr. Roux: Are you having a lot of pain with that left shoulder?
(Nancy, occasionally, like this weekend, I really did, and painkillers wouldn’t do anything for me.
(Dr. Roux: I’m not surprised by that. So, if you’re thinking of shoulder replacement, I’d suggest either a standard shoulder replacement or something called a Reverse total shoulder, which I don’t think you need.
Shoulder replacement can be quite effective at relieving pain, not always as effective at increasing motion. So for you, it’s really a very serious consideration, considering your heart, and that you could have potential serious, even life-threatening, complications that can occur with that.
(Nancy: How long does it take to recover from shoulder surgery?
(Dr. Roux, from a replacement, about 3 months. It’s not something I’m doing now – I do a lot of arthroscopic surgeries and I do knee replacements, but I don’t do shoulder replacements.
(Nancy: I was hoping for arthroscopic.
(Dr. Roux: Yeah, the arthroscopic procedure wouldn’t help you because you’ve got severe arthritis in there, so again, if you’re going to do surgery, it would be a replacement procedure.
If you wanted to consider that, I have three partners that do shoulder replacement commonly, (and we’ve done that on purpose, you know we want to have people doing it so they are doing enough of them a year, that they stay very current at it.) My three partners include Dr. Wong, Dr. Griffiths, and Dr. Orvald. They all do a fine job, and I’m happy to refer you for a second opinion, but I’m not sure that you want to, considering your cardiac status.
(Nancy: I think I’ll probably not. I’ve learned to compensate, but I guess I would like to know if I should not continue with Physical Therapy, because it isn’t going to help?
(Dr. Roux: It’s not going to help because it’s a mechanical problem with that arthritic joint. I would do what you are doing to maintain what you have, and if you started to lose motion, then I think physical therapy might be appropriate. Right now, I don’t think they are going to get any more motion with it because I think the primary problem with it is arthritis.
(Nancy: yeah, that’s what we were worried about.
(John: When you said you had pain this weekend, was that after playing your fiddle for 2.5 hours. (Nancy, yeah, and through a wind storm – it was crazy. (Dr. Roux, you were playing outside? I was up here covering the Central football game – it was blowing. (Nancy: yeah, it was! Also, I’ve been able to lift my arm up farther to wash my hair, after this physical therapy, but I still compensate. It’s not a big deal.
(Dr. Roux, I think you have compensated very well, and considering everything you’ve told me, I wouldn’t recommend doing a shoulder replacement.
(Nancy: Thank you. We appreciate your evaluation.
(John: One of her problems was when she had a heart blockage in 2009, she was scheduled to have the heart valve replacement in March of 2010, but she had the heart attack the day after Thanksgiving, in 2009…
(Nancy: and they took out the clot, successfully, but then the next evening, all my systems shut down and I was put on life support for 8 days.
(John: She had a reaction to Heparin, and she was in intensive care, flat on her back, and so her muscles… (Nancy: I lost all my muscles, even throat and stomach ones.
(Dr. Roux, “Sorry.” (Nancy, it’s okay, I got out of it.
(Dr. Roux, yeah you look good.
(John, so … this shoulder has bothered her a lot longer than that, but I think that time of total inactivity …
(Dr. Roux, on the shoulder, if you’ve got arthritis in there, and you have all that inactivity, it doesn’t respond well to the shoulder. All joints like to move; it helps nourish the joints, and so I’m sure a lot of your Chondrocytes (cells found in cartilage connective tissue) –> The cells in your cartilage die, and that contributed to your arthritis.
(Dr. Roux, You want me to show you that X-ray?
(Nancy: YES ! can I take pictures ? (Dr. Roux, yes.
Below, Dr. Roux’s evaluation provides diagnosis of my shoulder X-rays, 9-19-16:
 (Dr. Roux points out: You don’t have any joint space here anymore, and he continues with this question and comments.
(Dr. Roux points out: You don’t have any joint space here anymore, and he continues with this question and comments.
What are the signs of arthritis in a shoulder?
1. Joint space narrowing. You have joint space obliteration.
2. The other: Subchondral sclerosis, that’s where the bone is a little bit whiter on the socket side. You’ve got that.
3. Sometimes, you form Subchondral cysts, and you have them (cysts) on both the socket and the humeral head,
and,
4. Bone spurs (also called osteophytes). So really, you have all the signs of arthritis: Joint space narrowing, subchondral sclerosis, osteophyte formation, and cysts.
John and I have annotated my own photo of my X-ray below. I do not have the original X-ray image to work with, so this is a bit fuzzy, being captured from my video camera “movie” of Dr. Roux’s explanation.
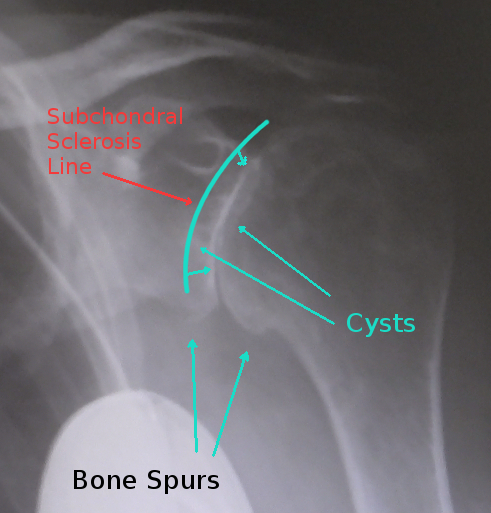
Subchondral sclerosis refers to the whitish line between the femoral head and the socket. Further, subchondral sclerosis is a disease that affects the bones and specifically the joints, of people who have osteoarthritis. Subchondral sclerosis causes joint pain and numbness (I have not experienced) by increased bone density and mass, and that produces a thin layer of bone beneath the cartilage in the joints.
John asked Dr. Roux if he had a normal shoulder X-ray to show us, but he did not have one on that computer. So, here is my attempt to compare:
 The left image is a normal shoulder I took from the web (from an Australian doctor’s explanation of shoulder arthritis). The right image is my left shoulder from the 9-19-16 X-ray. The big white spot in the lower left of mine is a metal ball hung around my neck for scale and density measurements. My image shows the obliterated joint space and the flattened head of the humerus bone on the bone of my socket. Note also the bone spurs protruding from the bottom sides of the two bones.
The left image is a normal shoulder I took from the web (from an Australian doctor’s explanation of shoulder arthritis). The right image is my left shoulder from the 9-19-16 X-ray. The big white spot in the lower left of mine is a metal ball hung around my neck for scale and density measurements. My image shows the obliterated joint space and the flattened head of the humerus bone on the bone of my socket. Note also the bone spurs protruding from the bottom sides of the two bones.
For further clarification of bone spurs (osteophyte formation), see the images below:
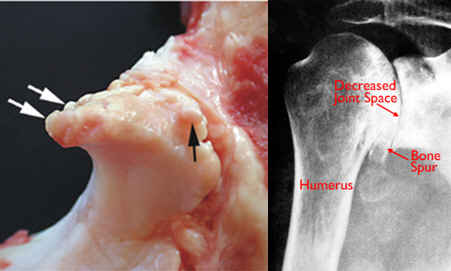 The left image is of a pig’s bone spurs (follow the arrows). The right diagram is of a human shoulder with annotations of the symptoms of osteoarthritis disease. (Osteo=bone)
The left image is of a pig’s bone spurs (follow the arrows). The right diagram is of a human shoulder with annotations of the symptoms of osteoarthritis disease. (Osteo=bone)
Wrap-up: Physical therapy is not an option, except if needed to maintain the slight range of motion I have gained since May. A complete shoulder replacement is potentially an option, but the surgeon (Dr. Roux) did not recommend because of the complications associated with my cardiac situation, which could be life threatening. I shall continue to do what I can, especially low impact and low aerobic exercising. Pain killers are not very effective, and because of being on Coumadin®, I cannot take the supplements often given for pain relief from joint arthritis (e.g., Glucosamine or NSAIDs [non-steroidal anti-inflammatory drugs] such as ibuprofen (Motrin®, Advil®) or naproxen (Naprosyn®, Aleve®). In addition, I am not allowed to partake of herbal and green tea solutions.
John quotes somebody: Getting old is not for sissies.
Tuesday, Sept 20
For Sept 19 CPAP. Reported figures. Time on 4 hrs 13 min with AHI=1.43. Events: 1 CSR, 6 H, 13 RERA. No mask leaks (max= 17 L/min). Oximetry: only on for three hours, and okay.
I reported in at 10:30 a.m. this morning to Natalie Joyce, owner of and therapist at Canyon View Physical Therapy. I took my printed transcription of what was said yesterday and carried my computer laptop to show her the videos of Dr. Roux’s analysis of the X-rays of my shoulder. She was grateful for the feedback. Much of it she had suspected from the work we had done on trying to increase my range of motion in several directions. When I left, they gave me a turquoise T-shirt, normally gifted at the end of a person’s time with them. We agreed to keep in touch. As well, if I realize I am backsliding on the gains with my ranges of motion, I will go back through my doctor for another referral to receive stretching sessions from the therapists there. I have worked with all the staff at Canyon View Physical Therapy (Ellensburg), and find them to be excellent, professional, and communicative about a person’s condition. They are pleasant and sincere educators and motivators. I send all of them a huge thank you commendation, along with my admiration, praise, and appreciation.
On my way home, I checked by Jerrol’s and got my $10 birthday present. I bought seven containers of 3-ring dividers to use for separation in the music books for our group. While there, I received instructions in how to make the white-out work that I bought earlier (in a tube). It needed squeezed just the correct way.
Wednesday, Sept 21
For Sept 20 CPAP. Reported figures. Time on 8 hrs 22 min with AHI=0.36. Events: 3 H, 16 RERA. No mask leaks (max= 13 L/min). Oximetry: looks nice entire time, with only one SpO2 blip to low of 88, all rest above, with avg 92.3%.
Today was a usual middle of the week activity. I normally pick up my friend, Gloria, and travel to the Food Bank for our singing with and for the audience, and afterwards we join a table for our lunch. Today was no exception but we grabbed some Starbuck’s day old chocolate chip cookies, and visited with some of the patrons, before the music. We eventually started at noon, and our youngest member, Kyle, brought his cigar box guitar that caused a lot of interest and discussion.
Thursday, Sept 22
For Sept 21 CPAP. Reported figures. Time on 7 hrs 6 min with AHI=0.99. Events: 7 H, 15 RERA. No mask leaks (max= 13 L/min). Oximetry: SpO2 one blip to low 85, a few below 88, with avg 91.6%.
Tried to finish the request for my medical records but did not finish before leaving for town. John drove so he could fill up his car for a long trip to Lake Serene tomorrow. I moved music stuff from my car into his.
We had nine people there today, plus Haley, our little dancer, and we had a good audience as well. My friend Clare returned my glass vase, and we carried a throwaway vase with beautiful gladioli for Jim and Lillian Brooks’ recent 69th anniversary. They carried them back to their apartment. Wheeled-Walkers are useful for such transport (even better for going through buffet lines).
I came home to work on dishes and computer issues and to put heat on my sore shoulder. Usually, I do moist heat before exercise and ice after.
Friday, Sept 23
For Sept 22 CPAP. Reported figures. Time on 5 hrs 11 min with AHI=1.16. Events: 5 H, 11 RERA. No mask leaks (max= 9 L/min). Oximetry: Fine all night.
I went to a CWU/Ruth Harrington scholarship luncheon today, donated my money for the year, had lunch, visited, and gave away a new shirt (still with tags) to a friend in the group. I realized my parking sticker expired 9/15/16, but I have to go across campus to renew it, so that awaits being done. I went directly to an exercise class at the senior center, and afterward, by Anne’s to water plants and pick up her mail. I stopped at a yard sale, where I found two nice plastic bins (with tops to keep the dust out) that have inside edges that hold hanging folders, so I can use them to encourage me to use my time saved from PT to get my monthly paperwork in order. My filing cabinets are filling. Yeah, I need to toss more stuff out of the ones we have in 3 rooms of the house. I already have recycled a lot, but there is a lot more to go. Amazing what >40 years of teaching will accumulate. I also found two containers: one I can use for John to carry his cell phone in, and protect it, and maybe he will not lose it. Another smaller one will work for my other cell phone.
On my way home, I dropped by a front porch to pick up a free gift of four unused lined journals that I can use in our cars to register tax deductible mileage for volunteer work and for medical trips. My Subaru Forester glove compartment is too small for the normally sold journals. John’s Subaru Outback’s is larger (go figure).
John was 130 miles away today working on the Lake Serene Trail near Index, WA. Actually, the trail is a 2-destination hike and the crew worked on the Bridal Veil Falls part. See:
They did not take the trail from the designated trailhead. Instead, they opened a nearby fancy gate (electric trigger and security camera monitored) and on a circuitous road through some nice small houses and then past your average meth-encampment – shacks and abandoned cars and trucks. The link above explains the trail and mentions the steps, as in the photo below.
You can get a better view from Google Earth than John had. It rained. Use the following coordinates in Google Earth:
47.789586, -121.569468
Zoom way in and realize you are looking down (and North). The Falls trail is on the west or left. The Lake trail crosses the stream at a lower elevation, then climbs up a slope until above the lake level and then comes back down.
 We did get some photos from today’s work party..
We did get some photos from today’s work party..
 Entire volunteer group came from MG2, an architectural firm, with this bunch all in a sector that designs Costco stores.
Entire volunteer group came from MG2, an architectural firm, with this bunch all in a sector that designs Costco stores.
Below is John with his crew with their stair-filling project. Rain and mist all day explains the whitish background of the left image.
This project was digging and filling to rehabilitate the steps, and to rock-in the sides to hold everything in place. After lunch they moved on.
 He called from Leavenworth at 4:35 and got home about 70 minutes later. We had leftovers for dinner.
He called from Leavenworth at 4:35 and got home about 70 minutes later. We had leftovers for dinner.
For me, much time this afternoon was trying to arrange to fill in music tomorrow at lunch for a conference at CWU, but no one was available, and I am not a sole performer. Maybe next year with more notice and not on the first weekend the nearly 12,000 students are back in town, we’ll be able to help. They needed someone to play from noon to 1:00 and payment was a free lunch.
Saturday, Sept 24
For Sept 23 CPAP. Reported figures. Time on 5 hrs 41 min with AHI=0.88. Events: 1 CA, 4 H, 23 RERA. No mask leaks (max= 10 L/min). Oximetry: Stopped from low battery 4.5 hrs in. SpO2 two blips to low of 89, all well above, with avg 92.9%. Total time sleeping was nearly 9 hours.
Nothing on tap today, except to cut John’s hair and work on the blog. I succeeded in cutting his hair.
Not all the dirty dishes got loaded, but the entire washer of clean dishes I unloaded. I spent most of the day on chores, the main one being this blog.
Sunday, Sept 25
For Sept 24 CPAP. Reported figures. Time on 7 hrs 28 min with AHI=0.13. Events: 1 H, 18 RERA. No mask leaks (max= 9 L/min). Oximetry: Good all night, except for several spurious finger changes recording in the 70s. Most were in the mid- to high nineties range (95-98).
John met neighbor Kenny in the morning to load a couple of bales of hay for him. He’s only recently out of the hospital with a 7-way bypass. He has 1 horse he will feed out of the truck for a couple of days and then let us know if he needs help loading again. John cut some brush and loaded it into the pickup, we ate, he napped, and now we have (nearly) completed this blog.
Nancy mixed in a few other chores but primarily worked on this report.
Hope your week was fine.
Nancy and John
Still on the Naneum Fan