Sunday, Dec 13
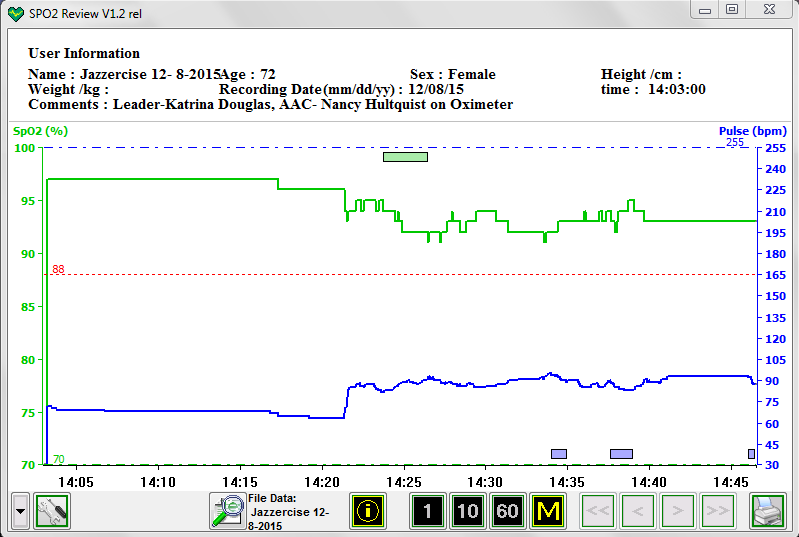
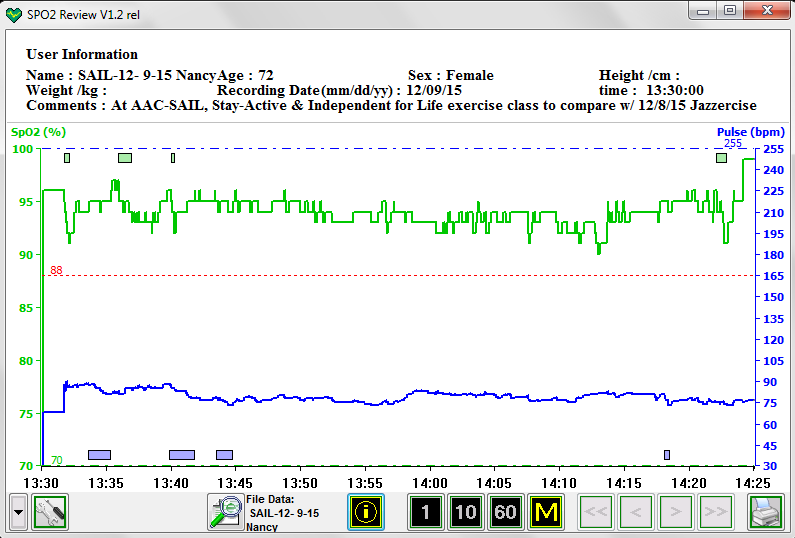
For Dec 12 CPAP. Reported figures. 5 hrs 50 min with AHI=3.60 Events: 21 H, 13 CSR, 13 RERA. No major mask leaks (max=20 L/min); oximeter NOT on an extra 3 hrs. I had on my older P-10 Air Fit. No clue what’s going on with the high AHI. Maybe was just congestion.
Nice dry sunny day, blue skies, and John stayed out to move the logs out of the pasture so the horses don’t tangle with them when they are snow covered. These are trees John felled to make way for the new driveway to access the back of our house with large equipment if needed (e.g., fire trucks) that cannot turn around in front of the house where we park. First use was the delivery of a load of fire-killed pines from just north of us.
I have continued working on updating our annual greetings list. I am finding an advantage for Facebook in this endeavor to contact people who have changed their email addresses from what we had previously. I finally managed at the end of today to notify all our email correspondents of the change in our computer domain.
Kitchen clean-up and then switching to den clean-up interspersing with computer work. Never really completed the needed den work.
I think we have agreed on Dec 30 for our annual Raclette this year at White Heron Cellars, in the Mariposa Vineyard, to thank the volunteer wine grapevine pruning crew. Now we can hope for decent weather. That is a Wednesday so I will have to miss my play date at the Food Bank that week and SAIL exercise.
Monday, Dec 14
For Dec 13 CPAP. Reported figures. 7 hrs 7 min with AHI=0.28 Events: 2 H, 2 CSR, 22 RERA. No major mask leaks (max=12 L/min); oximeter on an extra hr. with a lowered AHI and good activity the whole time, high SpO2. Top tube, from left to back of head, top of pillow.
Two horses trimmed, garbage bag of clothes packed to take tomorrow night to a family. Sunny outside, but <40° -- yet at John's brother's in CA it is 50°, and at his sister's in Cleveland, it is 60°! I sent out music to our group for January & February play dates around town, and made an announcement for this week to get a chair count. Today was pretty much a lost day for getting much accomplished.
Tuesday, Dec 15
For Dec 14 CPAP. Reported figures. 7 hrs 14 min with AHI=3.60 Events: 26 H, 13 CSR, 16 RERA. No major mask leaks (max=20 L/min). Bad night, no clue.
Up very early for me. Finished some music things; need to do more. I’m finishing a letter of recommendation for a student who took two classes in 2004 and wants to go to graduate school at the Univ. of Idaho, in the College of Natural Resources.
John found our heater for the horses’ water trough is not working. He is on line to find a replacement.
I have to shower and run music and clean up the stuff in den and go play music at rehab tonight. I did, and succeeded making it home in the snow, to a nice dinner John had prepared. It was Copper River salmon from Alaska.
Wednesday, Dec 16
For Dec 12 CPAP. Reported figures. 7 hrs 54 min with AHI=1.26 Events: 10 H, 4 CSR, 24 RERA. No major mask leaks (max=19 L/min); oximeter on an extra hr. with lowered AHI and good activity the whole time, high SpO2.
All the message for Wednesday disappeared, so I’m adding a little something here. Wednesdays always are the day I go to play music at the Food Bank, arriving at 11:30. Today was different, because I had to be at the hospital for a blood draw prior to noon, so the tests could be run for my INR and submitted to the surgeon for consideration of my dosage change of Coumadin prior to coming in the day of the surgery. Coumadin is a blood thinner, so it must be changed when they are cutting into my body. I went earlier than I needed, and it was a good thing, because just as I walked in the front door, the fire alarm was blaring, and I along with everyone in the lobby was asked to leave the building. We were out for maybe 5 minutes and had to stop people from entering. Never did know the cause, but I was told it was NOT a fire drill.
I checked in and proceeded back to the lab. I was told it would be 12 minutes at least before they could draw my blood. My blood was being drawn for 3 different doctors. Finally, I went in and it was done, but not before the fire alarm went off again. I left and drove to the Food Bank.
I was there early, but I checked the bread room and picked up a couple of loaves of bread. It was quite full because now the CWU students are on break, and the grocery store bakeries haven’t yet adjusted to fewer people in town. On inside where I helped set up for our music. We played, and then were served a thank-you lunch. We had 4 instruments and 8 singers. All instrumentalists there also sing as they play, until the Thursday group I play with.
From there to SAIL exercise class. That went well, and I came home by way of Grocery Outlet to buy mushrooms and frozen hashed-brown potato patties on a very good half-priced markdown.
Thursday, Dec 17
For Dec 16 CPAP. Nothing to report, except oximeter on and fine for 9 hours. My nose was too chafed to want to wear the mask and needed to get it better before surgery Friday.
Awoke to a couple inches of snow and more up to probably 5 inches, so poor John shoveled or swept off paths, driveway, and front yard. 95% was done with a push broom. Works well with powder-snow under 4 inches.

The image used is from the web – ours has a yellow plastic part where the handle (ole one broke, now use a metal conduit pipe) attaches. The plastic cracked today, so in need of repair or replacement. But, he “gotter done.”
I went to town over roads unplowed about 12 miles to play music. Only a few of us made it. We had 1 guitar, 1 fiddle, 1 flute, 1 tambourine, and 2 singers. Our audience outnumbered us. They were happy we came to play Christmas songs and wish them well. Their parking lot was not plowed. Happy I put on serious boots, and I will wear them tomorrow to the hospital in Yakima.
The UPS truck (with chains and 2 brown-suited young men) made a delivery late in the afternoon. Our drive was mostly cleared because we must get out early in the morning. The driver mentioned the easy access – they had a few places the chains were needed. One box had the horse tank heater and a kitchen timer. The other had a silicone cooking mat with indentions as big as those in a waffle – for chicken parts, rather than for things such as cookies. John didn’t have time to install the heater – the tank holds 100 gallons and is full.
Last minute prep, for surgery: I spent time talking by phone with a woman at the Yakima Memorial Hospital about their expectations for my defibrillator replacement surgery tomorrow, the times, paperwork, and things I needed to know or bring. I’m now getting things in order. We are expecting in at about 8 AM and out by 11.
Needed a copy of medications. Get to ER entrance, by 8:00 a.m. for check-in. John gets to accompany me to the room for set-up and then when they take me for surgery, he’s given a pager, sent to a waiting room, and called back when I’m back in the room. (That didn’t happen; he stayed in the prep room and read about the periodic table, or rather the discovery of each of the elements named therein.)
They will put me under “conscious sedation.” (from Merriam-Webster): Medical Definition of conscious sedation is an induced state of sedation characterized by a minimally depressed consciousness such that the patient is able to continuously and independently maintain a patent airway, retain protective reflexes, and remain responsive to verbal commands and physical stimulation—compare deep sedation.
I’m to remove my watch, but keep on my wedding band and my medic-alert bracelet. Paperwork is the normal photo ID and insurance proof. They provide socks, I keep on my underpants, but have to wear a typical hospital gown. I hope I don’t freeze. Biggest surprise is they will keep me for up to a couple hours after the surgery to give me something to eat and be sure it stays down.
I need to remember to ask about Tagaderm (Waterproof patches for over incision when I shower).
They will administer Penicillin for the antibiotic through my IV. I reminded them of my problem with Heparin, and she said none would be used in the IV or procedure.
We went to bed a little earlier than normal.
Friday, Dec 18 **HOSPITAL DETAILS**
For Dec 17 CPAP. no reported figures. I did not wear the mask nor my oximeter.
We left about 6:35 a.m. for Yakima Memorial Hospital to check in for surgery at 9:30 a.m. with Dr. Dao Pham to replace my ICD (Implanted Cardioverter Defibrillator). My battery ran out after 5.5 years.
I will try to report on the day’s excitement. I think we had over 8″ of snow here over the past two days. John had the drive and walkways swept. We got to bed relatively early for us last night. Roads in our valley were snow covered and it was dark. Some corners were slick. John drove my car, because it had been under cover and his (with newer tires) was covered with two days and nights of snow and sleet. We saw some cars off the road, but I-82 was basically plowed and sanded, but still a bit slushy. We made it to the entrance at 7:55 a.m. — so far, so good.
First trip was into an office to answer a bunch of questions and give signatures for the surgery procedure to be allowed to happen. I had already made a color copy of my photo ID (Driver’s license, Medicare and insurance cards), and handed a list of my medications (which that person didn’t want). “Save it for the nurse,” she said. I think that was all with her (10-15 minutes), and then we walked back to the front registration/lobby area, where a volunteer got a wheelchair for me. The reason escapes me, but it is the procedure. John had to walk – Destination: the “Cath Lab” – the Cardiac catheterization laboratory and services area. We did not learn the reason for the hospital policy for all patients to be wheeled in and wheeled out. Maybe it is because a person could get lost in the maze of intersecting hallways, side doors, and people milling about. The volunteer did the guiding and the wheeling.
She and I talked as we rolled along. We finally got there and I was taken into room #3, across from one of the cath labs where the procedures such as mine occur (not the one I eventually traveled to).
Then the fun began. John was with me and would end up staying there – against the wishes of the area supervisor, but the nurses didn’t care. They had me undress and brought me a potty to use before getting into my gown, socks, and under two heated cloth covers (called blankets). After I redressed, and hopped into bed, the stuff began. First, a guy (Sam) came pushing a rolling table and then placed an instrument that looked like a short printer on the table. He introduced himself as being with the Boston Scientific company, the maker of the ICD I was about to have join my body parts. He needed to read the data off the Biotronik unit still in my body to store in the new unit, so there was a smooth turnover of data on my heart. He had to wait until a nurse (PJ) got me all hooked up to nodes for an ECG/EKG during my surgery, and she connected a blood pressure cuff to record that with my vitals every few minutes. She put an oximeter on my finger (to read my pulse and SpO2); I am not sure how my respiration was being measured and recorded, but she took my temperature and started the recorder. The system was not cooperating, so nurse PJ (who was to be my scrub nurse in the operating room) left for someone with computer savvy to try their hand at it. She fixed it. John was facing the screen (and it was behind me), so he kept me informed about my vitals.
The next step was to have another person come in to set up the place on my arm for IV entry of the antibiotic during the 45 minutes preceding the expected surgery at 9:30 a.m. Her name was Nancy. She seemed to find the vein well, but the needle apparently was hitting a nerve and hurt me the entire duration. Once she got it placed, there were two connectors, one for input and the other for withdraw. She needed to take blood to check my INR before the surgery. It was down to 1.7. That was down from missing only one Coumadin 2.5 mg pill the afternoon before. Wednesday morning 2 days earlier, the INR was 2.4. As nurse Nancy was leaving, she asked if I had any more questions about what was to happen in the procedure, and I said, “Yes, when can I expect to be taken into the Cath lab for preparation there for my 9:30 scheduled start of the procedure, (setting me up on the operating table, scrubbing, infusion of the sedation, and whatever.). She paused and said, “Well, the doctor has been delayed, and there are two people ahead of you, so I estimate it will be about 11:00 a.m.” WHAT ?? It is too bad my vitals were on Standby at the time, because I am sure my BP rose significantly. Why the heck didn’t someone tell me sooner? I wonder when we would have been told anything, had I not asked her the question as she was walking out of the prep room.
John and I wondered out loud what had happened. It was 8:45 and I could watch the clock above his head. He and I talked awhile and I covered myself with a second warm cover, and tried closing my eyes to relax, hoping to forget the pinching pain of the IV needle (IV not yet hooked up). I decided if I turned my hand backwards, it took off the pressure some.
A new cheerful young nurse appeared, named Sarah. Both she and PJ were going to be with me throughout the whole procedure. I asked her if she had any idea what had happened to delay the operation. She said she didn’t know about it, as she had just arrived at work (not even clocked-in yet), and she would go find out and report back. She returned shortly to say it would be a little while until the doctor arrived, that he was returning from Seattle last night, and got stopped/stranded on Snoqualmie Pass and spent the night sleeping in his car. [John knew avalanche control crews closed the highway during the night.] He had made it back to Yakima and was on his way to the hospital. At least we now knew something. So, she told me would check back in and keep me up on things. She brought me another warmly heated cover. The room we were in had curtains for its door, so while we couldn’t see who was outside, I could hear all the conversations, even from the supervisor’s desk around the corner.
I relaxed, John read, and I listened to all the conversations. I heard the staff talking about the really good fudge someone brought in to share. I heard Dr. Pham’s voice when he arrived, and his telling the story about his crazy night. I heard my two nurses outside the door talking about their husband’s foot injuries. I continued resting. At some point Sarah returned, hooked up my IV, and told me rather than Ancef, I would be receiving Vancomycin, a stronger antibiotic. I had her bring me another warm cover, because it was chilly in the room. (It was even chillier once I got to the operating room.) John was watching the flow of the IV and keeping me in the know. At some point in that process, Sarah again came in to check. I told her about the pain at the needle entry, and she felt my arm above my wrist to be sure it was entering properly and not sending the IV fluid outside my vein. It was all right, but she went away and brought back a heating pad for the insertion point, and it really did help. Finally, I heard the door across from me open (to the other Cath lab), and I recognized Dr. Pham’s voice, as he was going in for the person’s surgery ahead of me. All of his patients this morning were relatively simple exchanges, with no new wire leads being inserted into the heart chambers. Not too much time passed before Sarah came to get me to go to my Cath lab for last minute preparations. I jokingly said, “Please grab me a piece of that yummy sounding fudge to go with my meal after surgery.” She said she would (and she did !).
She asked if I could walk on my own. I was happy to do that. We walked about 25 feet, I guess. I entered the big room and climbed up on a little step stool to get on the operating table. Three attendants stayed busy setting me up. I requested another pillow for my head and one for my left arm. I was able to watch the screen with my vitals. At some point, they added oxygen enhancement in my nose and I saw the SpO2 increase to 100%. John had told me it was 97 to 98% in the prep room, and I breathed deeply a couple of times to increase it to 99%. My BP was fine the entire time.
Another person, Presa, took over for Sam with the Boston Scientific equipment. One thing she had to do was to magnetize the old unit to take away its ability to shock, so that we would not set it off during the removal procedure. Good idea! They continued working on me, building up to the final scrubbing with, I guess, some high-powered disinfectant on the part of my skin to be cut. It was a very wet process, and it left ugly green stains all over my neck, upper body, and shoulder. On the other side, Sarah, warned me she was putting a very cold item on my abdomen. It serves as a ground. Finally, SJ covered my incision-to-be area and taped me in. She had me turn my head away to the right, to prevent any contamination. Eventually, my face and eyes were covered with a blue tarp like covering. My head already had a cap from the original prep room. Finally, the doctor arrived and our conversations continued. Nurse Sarah asked me to tell her my name, birth date, and why I was there. I obliged. I joked with the surgeon, and told him I heard he had a rough trip back across the pass, and I was happy I was third in line, so he’d had a chance to wake up. He laughed and said he got very cold sleeping in his car, but he was okay. He began making the incision with a scalpel. I heard another strange noise, and asked what the sound was. He said, “A cauterizer.” I said, “Oh, to stop the bleeding,” and he agreed. He opened me and managed to get the unit out without too much pushing around. At one point, he commented he was examining the pocket. There was enough moving and pushing that I knew I would be sore afterwards. Acetaminophen every 6 hours has handled it. Another noise of riveting ensued when the wire was removed, and then reinserted into the new unit. I commented and that was acknowledged, as well. The new unit is about the same dimension in length, but it is thinner. They gave me my old unit as a keepsake. I think I will take it to my device check appointment Dec 29, and take a picture of it beside a like unit that is now part of me.
Dr. Pham sewed me up, put on strips over the sutures, and covered it. Then they took off the cover over my head, and I saw him for the first time. I said, “Hi, Dr. Pham, welcome back to Yakima, and thanks for doing my surgery.” We then talked a little more about his trip. He actually had flown to Belgium to pick up a relative to bring back to Seattle. That was his vacation. I mentioned the weather had been bad in Europe, and he said, “Yes, it was. It rained the whole time I was there.” Then he left and the nurses moved me to the stretcher to go back to the prep room. I asked if I could walk back. No. I should have asked them to raise the stretcher higher. There was a 4-6″ drop I had to make to move from the operating table. I would have preferred they let me step off the table and get back into the bed, to be rolled back to the room, if I wasn’t allowed to walk. So we got back and I said hi to John. We agreed that it took longer than we anticipated.
We were talking and one of the nurses came in to give me the final orders, and then she was followed by Dr. Pham. While he was in the room, Sarah brought me the piece of fudge I had wanted. The surgeon said he wanted a piece too, so she went back for his. He told me I had no restrictions, except I couldn’t shower for 3 days, and I needed to let them know if I had any signs of infection. The covering tape and gauze protecting the major cover needed to be removed tomorrow. The other was not to be gotten wet, and would be removed and the red & silver slips underneath the patch, but over the sutures, would be removed by the device technician, Dec 29th. He told me to withhold aspirin until Monday (48 hrs) and to resume Coumadin tonight. He bid us adieu.
We had food – a drink and leftovers of chicken & shrimp and dried apples. Now it was 12:15. A staff member asked if I could sit on the side of the bed to eat. I did. She rolled the table over with a tray of food: a half of a large turkey sandwich with 3 pieces of bread and 2 large pieces of dark green lettuce. I took off the lettuce (I’m not supposed to intake Vitamin K) and the middle piece of bread, added mayonnaise, and ate it. A cup of fruit had one slice of orange with a peel and the rest of the cup was without peels, but sectioned nicely. I tasted one without a peel, and asked John to taste one. It tasted like grapefruit to me and to him. I pushed the “light,” the nurse arrived, and I asked her if it was grapefruit or orange and she said all was orange. I hesitantly ate the rest of the slices. One of my medications prohibits grapefruit. I still don’t think it was orange sections. There was a cup of coffee, but it was cold. I imagine my lunch was ordered for the old schedule of the operation to be over at 10 or 10:30, and this was two hours later. There was a very large cup of water that I drank. Once I was done eating and dressed, I could leave. However, they had to wheel me out in a wheelchair. I asked for some Tagaderm patches to over my incision dressing when I showered. The assistant pushing me out found me some on the first floor in a storeroom. If I need more, I will go by the hospital here and ask, next Wednesday, when I go in for my INR check blood draw to see if my value returned to where it is supposed to be.
On the way home the roads were fine, although we did see a car that had gone skiing off to the right on a long downhill section. The car had gone off where there was a gentle dip with no guard rail. After the dip it went upslope a little, then down again and was resting against the outside of the (now present) guard rail. Wish we had a photo of that but it wasn’t the time nor place for one. We assume the retrieval will require a heavy lifter.
When we got home we heated leftover pot roast.
Saturday, Dec 19
For Dec 18 CPAP. Reported figures. 7 hrs 50 min with AHI=0.64 Events: 5 H, 0 CSR, 10 RERA. No major mask leaks (max=17 L/min). Oximeter report good. I wore my Dreamwear top tube mask, and the tube went across my body, to the top, and over my right shoulder.
Today started with a request for firewood from a friend of at least a decade. John went out and drove the pickup truck around making paths so she could survey the various stacks of wood. Her 4WD Expedition had good tires so that allowed them to eliminate a truck-to-SUV transfer and saved time and work. She does have an old pickup that would have held more, but it does not have a back (or crew) seat section and thus isn’t legal for kiddy transport. After the loading, she took a photo. {RIGHT Click, select ‘New tab’ on images to get proper aspect.}

We had a nice sunny day, but while the loading took place, a fog moved over, as seen in the top right corner of the photo. No matter, she had about as much wood as she could get and was on her way–about 20 minutes to home. She reported back a thank you later on Facebook that she he unloaded it, split some, and started a fire in her wood stove, increasing the temperature from 55° to 68°. Nice for the family, with three little girls under the age of 8 (the oldest is 7).
Now back to body parts. I managed to remove the surgical tape covering the incision-protecting pad below my left collarbone. It was two overlapping strips with gauze protecting the main cover of the sutures, and was cumbersome — two strips about 6″ long and 3″ wide, each. At the hospital, the material wasn’t staying in place very well. A nurse applied something sticky (& brown) under the corners and edges. That was all that needed to be removed today. I succeeded, so likely it wasn’t Gorilla glue.
I wrote a story for another request on the BNE site, and next Wednesday, I will be picking up a nice pair of lined suede boots and leggings to keep me warm. I plan to wear them to the wine & Raclette festivity scheduled for Dec. 30, midday.
I took a couple of photos of the snow, icicles, and Rascal.
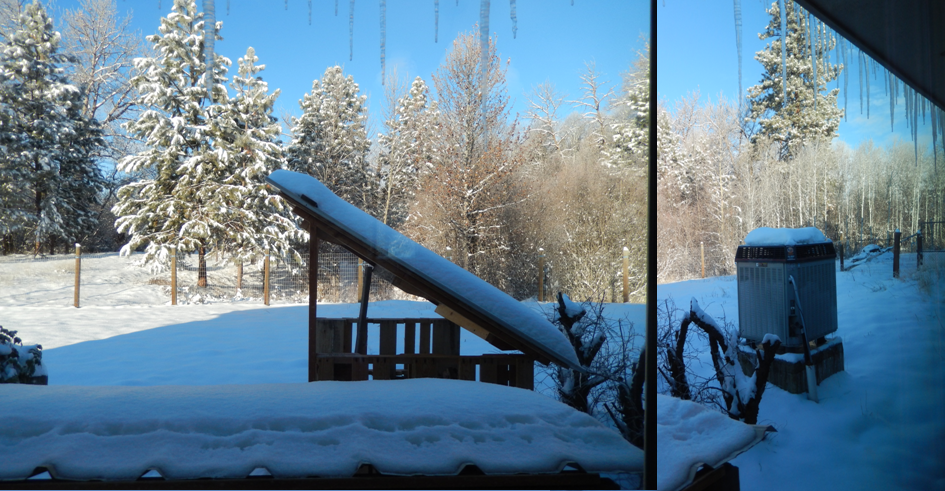
This collage above shows photos taken out the new patio door. Left shows two structures with metal roofs, the closest to keep roof runoff from splashing on the new outside (unfinished) door. Drip line shows in the snow in front. On the back side on the patio are 5-gallon buckets to catch the snow melt or rain. The back structure on the left is the protected wood pieces for our stove. On the right is our heat pump and both photos show hanging icicles.

Above is from our bedroom window looking back to the cat’s mow, and the outhouse-looking feature that serves as the heated “cat house” for our 3 outside feral cats. The cat in this picture is Rascal, our inside-outside cat. In the right photo, between Rascal’s right ear and the hay mow, is the location where John has some piles of cut wood (he gave from this morning). See above.
I spent a lot of time on emails today and working on the blog, but it is not yet finished to go through John’s editorializing. Perhaps in the morning when it is too cold and snowy to be outside, after morning feedings.
John fixed supper with the frozen chicken I bought last week, and mushrooms this week, and some canned Pineapple rings and Butternut squash (not ours, but “fresh”).
Sunday, Dec 20
For Dec 19 CPAP. Reported figures. 7 hrs 41 min with AHI=1.17 Events: 9 H, 2 CSR, 21 RERA. No major mask leaks (max=19 L/min); oximeter on entire time, no longer with good activity the whole time, on SpO2.
Awoke to snow, falling hard, while John fed Woody (after she appeared on her perch on the cable table). I took a picture from the front door, and then he took the food plate out to put under his car where she was more protected from the snowfall. More explanation is below the collage, next.

Woody sitting on the cable table inside our front fence, waiting to be fed. This is a morning ritual. Evenings she normally eats out back with the other two ferals, Lemon and Sue. Middle above she is watching John walk through the front gate to put her food dish under his Subaru for protection. Right photo shows her headed to eat.
We are now getting ready to sit down to pizza for lunch, and then John will transfer this to WordPress, I will proof again, and we will publish later this afternoon.
Hope your week was fine.
Nancy and John
Still on the Naneum Fan